The Institute Colloquium: Predicting future evolution: experimental approaches, pract
Date
Monday, October 14, 2013 16:30 - 17:30
Speaker
Barry G. Hall (Bellingham Research Institute)
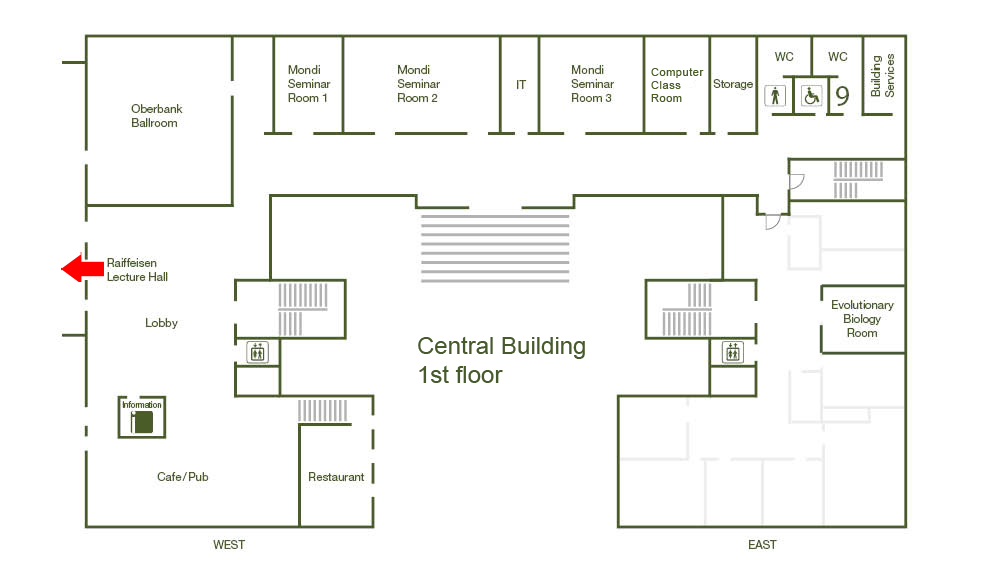
Location
Raiffeisen Lecture Hall, Central Building
Series
Colloquium
Tags
Institute Colloquium
Contact
Every year influenza vaccines are based on attempts to predict the short-term evolution of the influenza virus. Hospitals try to predict the evolution of antibiotic resistance genes and to cycle the use of antibiotics in an effort to slow down the local evolution of those genes. Those efforts are usually unsuccessful. To reliably predict the evolution of pathogens we must understand evolution as a process, understand the constraints on that process, and frame that understanding in a way that permits practical application of what we have learned. I will discuss three experimental studies designed to inform us about the evolution of new functions and to allow us to predict evolutionary outcomes. (1) The EBG system followed the genetic, biochemical and molecular changes involved in the evolution of a new lactose utilization system in E. coli. A specific, branching, evolutionary pathway was demonstrated that led to a greatly expanded substrate range and a 20-fold increase in lactase activity. (2) Point mutations that increase activity are one way that organisms can acquire new functions. The can also evolve new functions by expressing normally silent operons that include several genes that are required for the new function. E. coli cannot utilize ?-glucoside sugars, but it possesses three separate silent, or cryptic operons that when activated, often by spontaneous insertion of mobile elements, allow the strain to grow on those sugars. (3) We developed an in vitro evolution system to predict the evolution of the TEM ?-lactamase antibiotic resistance genes. After showing that our system faithfully mimicked natural evolution, we applied our system to predicting how TEM would evolve to confer resistance to a new antibiotic, cefepime. At that time, in nature, no TEM variant conferred clinical resistance to cefepime. We evolved variants that conferred very high resistance, and predicted the exact pathway of amino acid substitutions needed to achieve the highest level of resistance. One of those substitutions was already present in a variant that conferred sub-clinical resistance. Two years later the predicted second-step mutation was found in a new TEM variant that conferred clinical resistance